Introduction
When a patient arrives with multiple ICD shocks in quick succession, the room fills with urgency. For electrophysiologists, this isn’t just another case—it’s a battle against one of the most feared arrhythmias: Ischemic Scar Ventricular Tachycardia (VT) Storm.
This blog takes you inside the journey of a 52-year-old man whose relentless VT episodes were finally silenced through advanced 3D mapping and radiofrequency ablation (RFA).
The Patient Story
A 52-year-old man rushed into the ER, terrified and exhausted. His ICD had delivered multiple shocks, each one a brutal reminder that his heart was trapped in chaos.
-
Past history: Old anterior wall myocardial infarction (AWMI)
-
Device: ICD implanted for secondary prevention
-
Current findings:
-
Echo revealed severe LV dysfunction (EF 30–35%)
-
ICD interrogation showed VT Zone 2, HR 180–200 bpm, multiple ATPs and shocks
-
The plan was clear but challenging: Scar modification using 3D-guided EPS + RFA.
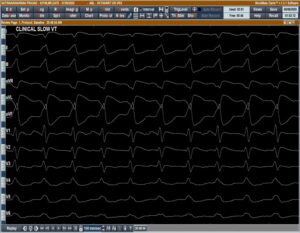

ECG Insights: The First Clue
The baseline ECG hinted at basal anterolateral LV VT. But something unexpected happened—once the RV catheter was placed, the VT terminated.
This provided a golden opportunity: to dive into mapping the slow zones responsible for sustaining the arrhythmia.
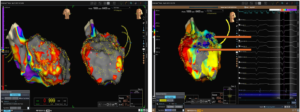
Mapping the Heart’s Hidden Maze
Scar mapping revealed a bleak picture—extensive scar tissue blanketing the anterior wall, anteroseptum, and anterolateral wall.
ILAM mapping added another layer of clarity, showing two critical deceleration zones (DZLs)—the likely culprits behind the re-entrant VT.
A Dangerous Turn: VT Induction
When VT-2 was induced during the procedure, it quickly degenerated into a faster, unstable rhythm.
The patient’s blood pressure plummeted. Immediate cardioversion restored sinus rhythm—reminding everyone in the lab of the razor-thin margin in scar VT ablation cases.
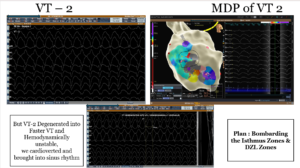
Ablation: Bombarding the Isthmus
The ablation strategy was aggressive yet precise:
-
Target the isthmus and DZL zones
-
Identify and eliminate late potentials
-
Apply RFA lesions to block every possible re-entrant pathway
This was like sealing off escape routes in a maze—until the VT had nowhere left to run.

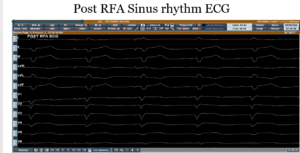
Victory: Silence After the Storm
After the ablation, repeat induction was attempted—no VT could be induced.
The patient’s heart settled into a stable sinus rhythm. The ICD remained quiet. For the first time in days, his heart was at peace.
Key Takeaways
-
Advanced 3D mapping and ILAM-guided ablation are game changers in scar VT management.
-
Targeting isthmus and slow conduction zones is critical for success.
-
Even in patients with severe LV dysfunction, well-executed RFA can transform outcomes.
This case is a reminder that with the right tools and expertise, even the fiercest VT storm can be silenced.
Frequently Asked Questions (FAQs)
1. What is scar-related ventricular tachycardia (VT)?
Scar-related VT is a dangerous arrhythmia caused by electrical re-entry circuits forming around scar tissue in the heart, usually after a heart attack. It can lead to palpitations, fainting, or even sudden cardiac arrest if untreated.
2. Why do patients with ICDs still get shocks?
ICDs save lives by detecting and terminating dangerous rhythms, but they do not prevent arrhythmias from happening. If the scar tissue keeps triggering abnormal circuits, patients may experience recurrent shocks, which are painful and distressing.
3. What role does 3D mapping play in VT ablation?
3D mapping allows cardiologists to create a detailed electrical “map” of the heart, identifying scarred areas and slow conduction zones. This helps in pinpointing the exact regions responsible for VT, guiding precise ablation.
4. Is VT ablation safe?
Yes, in experienced hands, VT ablation is considered safe and effective. While all heart procedures carry risks, ablation reduces ICD shocks, improves quality of life, and in many cases, prevents future VT storms.
5. How successful is VT ablation?
Success depends on the extent of scar and heart function. In many patients, ablation significantly reduces or eliminates VT recurrence. As in this case, post-RFA, no VT could be induced—showing a strong procedural success.
6. What is the recovery like after VT ablation?
Most patients recover quickly, often discharged within a day or two. Fatigue is common for a short period, but overall quality of life usually improves as ICD shocks decrease. Regular follow-up is important.
7. Can VT come back after ablation?
Yes, there is always a chance of recurrence, especially in patients with extensive scar tissue and poor heart function. However, repeated ablation or device optimization usually helps manage such cases effectively.
8. Who should consider VT ablation?
-
Patients with recurrent ICD shocks
-
Those with symptomatic, drug-resistant VT
-
Patients with VT storm (multiple episodes within 24 hours)
A cardiologist or electrophysiologist decides based on individual risk and benefit assessment.

